#20 CRRT w/ Dr. Kevin Chung
On this week’s episode of Critical Care Time, Nick and Cyrus discuss continuous renal replacement (or kidney replacement) therapy and acute kidney injury with master intensivist and extra corporeal aficionado, Dr. Kevin Chung. Dr. Chung is a retired colonel in the United States Army, the principal force behind an intensivist-run renal replacement program in San Antonio, and is currently the Chief Medical Officer for our season one sponsor, Seastar Medical.
In this episode, we discuss an approach to acute kidney injury, demystify elements of continuous renal replacement therapy, and then discuss various applications to include blood purification technology in 2024.
Quick Take Home Points:
Renal replacement therapy is a life saving intervention in the ICU. Continuous Renal Replacement Therapy (CRRT) has advantages over other forms of renal replacement (IHD, SLED) among people with critical illness.
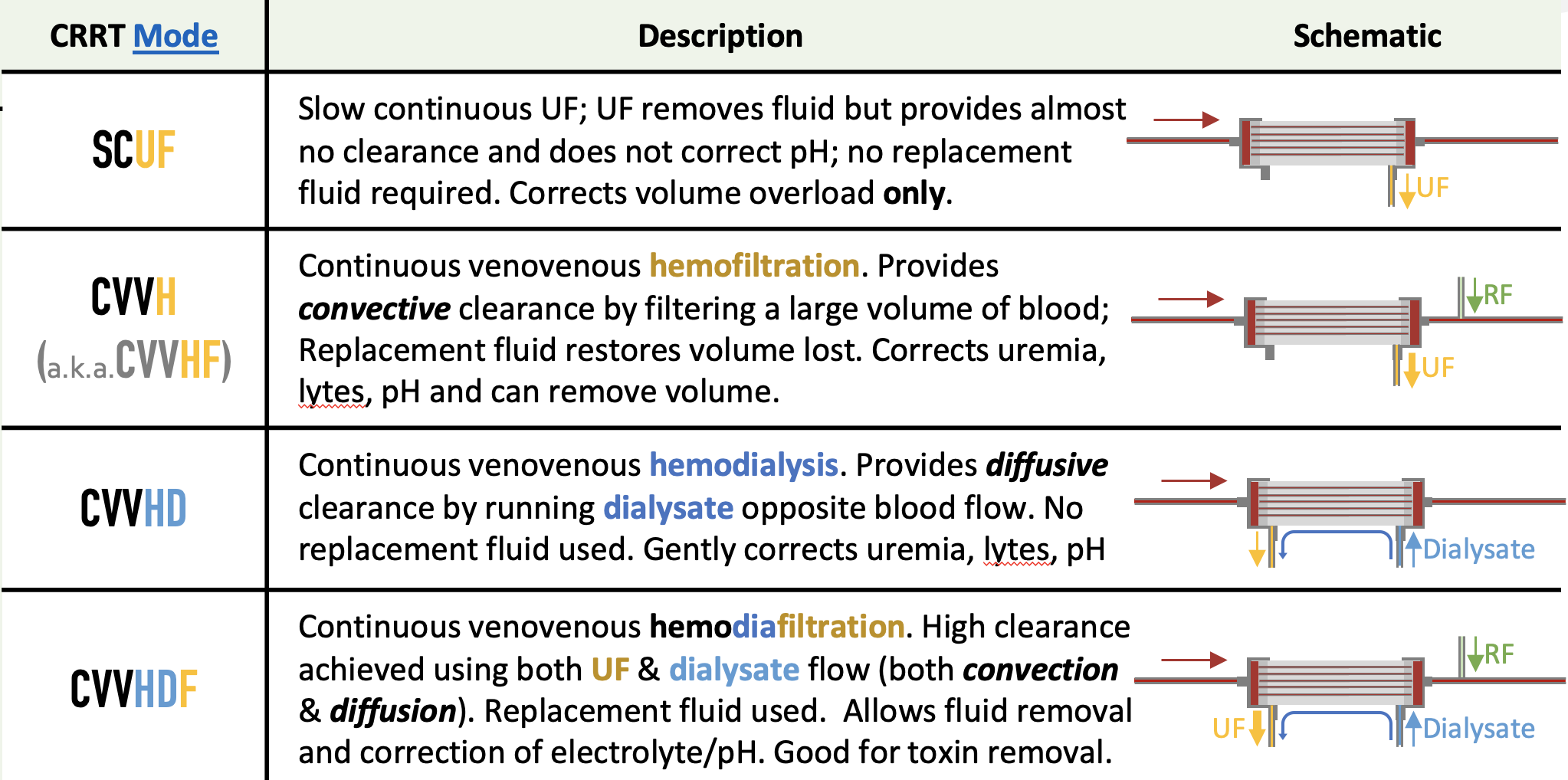
Different modalities of CRRT are available: SCUF, CVVHF, CVVHD, CVVHDF. Understanding convective vs diffusive clearance is important to understand the advantages of each.
CRRT is often interrupted, which can lead to under-dosage. Anticoagulation with citrate is an important strategy to maintain filter patency and avoid interruptions.
Blood purification technologies are an emerging technology that can be combined with CRRT to remove inflammatory mediators such as
Show Notes:
The Basics
Acute Kidney Injury is common among people with critical illness. Depending on the definition used 30-60% of ICU patients experience Acute Kidney Injury (AKI) and 10-15% require renal replacement therapies. Despite its frequency, outcomes of AKI requiring renal replacement therapy are poor, with >50% mortality in many studies.
Renal Replacement Therapies (RRT) are used in patients in the ICU with renal failure to remove excess fluid or to clear the blood of toxins (such as urea or potassium).
Clearance (K) is the volume of blood cleared of a solute (typically urea) per time. Clearance depends on Blood flow (QB), dialysate flow (QD) and the dialyzer.
There are two primary mechanisms that contribute to clearance::
Diffusion (predominantly with dialysis) clears smaller molecules (<200 D). Concentration gradients are used to acheive dialysis.
Convection (predominantly with UF) clears small & medium sized (< 50kD) molecules. Pressure gradients are used to achieve ultrafiltration.
Different types of Renal Replacement Therapy are available in the ICU, which typically depends on institutional preferences:
Intermittent Hemodialysis (IHD)
Slow Low Efficiency hemoDialysis (SLED)
Continuous Renal Replacement Therapy (CRRT)
Comparison of modalities used for renal replacement therapy in the ICU. Source: ICU OnePager
The CRRT Circuit Explained
ICU OnePager infographic about RRT in the ICU. Credit: Nick Mark, MD 2021
Components of the CRRT circuit include:
The DIALYZER is rigid case that encloses thousands of semi-permeable polymer tubules. Blood flows through the tubules & dialysate flows in the opposite direction outside (countercurrent).
Dialyzers differ in surface area (m2), hydraulic permeability (KUF), permeability to medium sized molecules (flux of β2 microglobulin), & permeability to small molecules diffusion (mass transfer coefficient). For simplicity, we often refer to dialyzers as either HIGH FLUX or LOW FLUX.
DIALYSATE is a the fluid that flows through the dialyzer outside of the tubules that contain blood. Dialysate flows in the opposite direction as blood, which generates a countercurrent. Dialysate is often selected based on the patients blood chemistries.
For example, to correct hyperkalemia a low K dialysate is used and vice versa.
DIALYSATE FLOW RATE (QD) is the flow of dialysate through the dialyzer. Higher flow rates enable greater clearance of small molecules via diffusion.
BLOOD FLOW RATE (QB) is the flow rate of blood through the dialysis circuit. Higher flows enable greater clearance/UF & has lower thrombosis risk but may require larger access & have more adverse hemodynamic consequences. Low blood flow is “gentler” hemodynamically but acheives lower clearance and has greater risk of thrombosis.
REPLACEMENT FLUID (RF) can be used to restore fluid volume removed by UF in the dialyzer. Replacement fluid can be given pre- or post-dialyzer
ANTICOAGULATION may be used to reduce thrombosis in the circuit. Two options exist:
Heparin (may be reversed with protamine)
Citrate (usually reversed with calcium) - typically the superior option.
VASCULAR ACCESS can be permanent (such as an AV fistula or an AV graft) accessed using needles, semi-permanent (a tunneled CVC), or temporary (such as a non-tunneled CVC).
For continuous renal replacement either a tunneled HD line or a temporary HD must be used. For Intermittent HD an AV fistula or graft can be used.
NB: The “arterial” (red) side describes blood coming out of the patient; it does NOT mean that it comes out of an artery.
ULTRAFILTRATION (UF) is the filtration of water from the blood, driven by the transmembrane pressure (TMP) gradient between the blood & effluent. TMP can be titrated by adjusting the effluent pump & pressure. Ultrafiltration (UF) provides clearance by convection (also called solute drag) removing small & medium sized molecules.
DIALYSIS is a the removal of molecules from the blood driven by a concentration gradient between blood and DIALYSATE.
Continuous Renal Replacement Therapy (CRRT)
Why CRRT?
CRRT has the advantage that it is hemodynamically gentler than other forms of RRT. This means that it may be better tolerated in people with critical illness.
There is some emerging evidence that CRRT may be associated with better renal outcomes that IHD, particularly in certain populations (intracranial pathology).
CRRT is usually run by ICU nurses, which can make it easier to initiate (no additional staffing required). Because CRRT uses sterile fluid the material costs are higher, however the staffing costs may be lower, making the total cost roughly equivalent.
IHD can deliver more clearance faster, which is potentially advantageous when rapid removal of toxins is required (e.g. overdose).
CRRT can be combined with ECMO using the same vascular access.
Modes of CRRT:
SCUF - uses a pressure gradient to provide ultrafiltration only. This is useful for correcting volume overload but provides minimal clearance.
CVVH / CVVHF - uses a pressure gradient to provide a large amount of ultrafiltration. Removal of such a large volume of fluid provides convective clearance due to SOLUTE DRAG. Because so much fluid is removed REPLACEMENT FLUID is added to restore lost volume.
CVVHD - uses the countercurrent flow of DIALYSATE opposite the flow of blood to provide diffusive clearance.
CVVHDF - combines a pressure gradient to generate UF and countercurrent flow of dialysate to provide dialysis. The combination diffusion and convection provides a large amount of clearance.
Importance of Dose
Adequate dosage is crucial, and under-dosage of CRRT may be associated with worse outcomes. Several studies have found that the dose actually delivered is far less than prescribed. (For examples, one study found that patients typically received 60% of the intended dose.)
Interruptions in CRRT cause under-treatment. Some of these interruptions - such as clots in the circuit - can be prevents, such as with anticoagulation.
Other interruptions (machine alarms, catheter dysfunction, bag/tubing changes, or deliberate disconnection for radiology procedures) are harder to mitigate.
One approach is to deliberately prescribe a higher dose to compensate for an anticipated 15% circuit downtime.
Just as important as the dose of RRT is adequately dosing medications for people undergoing renal replacement.
Many medications - including antimicrobials - are removed by the CRRT circuit. Promptly adjusting dose of medications when someone begins CRRT is crucial to prevent treatment failure.
CRRT also affects nutrition, since amino acids are removed by the dialyzer. Higher protein dose is necessary to offset this.
Timing of initiating renal replacement therapy
Evidence from multiple RCTs suggests that initiation of renal replacement therapy prior to the onset of organ failure may improve clinical outcomes.
Blood purification technologies
Several technologies have been developed (or are in development) for extracorporeal blood purification in critical illness. These are often uses in conjuction with CRRT. The concept is that removal of inflammatory mediators can reduce ongoing inflammation and mitigate organ damage.
Several techniques are available:
Convection techniques - purify blood by ultrafiltration.
Examples: High cut off membranes (HCO), high volume hemofiltration (HVHF)
Absorption techniques - purify blood but binding target molecules
Specific absorption techniques removes only targeted molecules.
Examples: Polymixin B (PMX), LPS absorption
Non-specific absorption techniques
Examples: Hemosorption (e.g. Cytosorb)
Combined techniques -
Combined filtration and absorption (e.g. oXiris)
Coupled plasma filtration absoption (CPFA)
Plasmapheresis
Selective Cytopheretic Device - an investigational device that targets activated leukocytes, which are the cellular sources driving a hyperinflammatory process.
Episode Outline
06:22 Intensivist-led CRRT Programs; collaboration with Nephrology
08:42 Approach to AKI in the Critically Ill Patient
15:14 Prevalence of AKI in the ICU
20:32 Biomarkers for Early Detection of AKI
28:11 Approach to AKI Stage
34:54 Introduction to CRRT
35:22 Introduction to CRRT and its Components
36:46 Overview of CRRT and its Uses
43:34 Different Modalities of CRRT
48:42 Comparison with Intermittent Hemodialysis
53:00 Considerations for Anticoagulation
57:25 Importance of Dose in CRRT
01:01:37 Timing and Duration of CRRT
01:06:00 Cost and Alternative Uses of CRRT
01:10:59 Comparison of CRT and intermittent hemodialysis
01:11:45 Hemodynamic shifts and kidney injury
01:13:50 CRT contraindicated for TBI patients
01:14:18 Timing of initiating renal replacement therapy
01:19:05 Anticoagulation in CRRT
01:24:08 Cost considerations of CRRT
01:29:39 Timing of ending CRRT
01:32:26 Blood purification technologies
Audio
Video
-
Pickkers P, Darmon M, Hoste E, et al. Acute kidney injury in the critically ill: an updated review on pathophysiology and management. Intensive Care Med. 2021;47(8):835-850.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012;2:1-138.
Zarbock A, Kellum JA, Schmidt C, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA 2016;315:2190-9.
The STARRT-AKI Investigators. Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. N Engl J Med 2020;383:240-251
Gaudry, S, Hajage D, Benichout N, et al. Delayed versus early initiation of renal replacement therapy for severe acute kidney injury: a systematic review and individual patient data meta-analysis of randomised clinical trials. Lancet 2020;395:1506-1516.
Naorungroi T, Neto AS, Wang A, et al. Renal outcomes according to renal replacement therapy modality and treatment protocol in the ATN and RENAL trials. Crit Care 2022;26:269.
Continuous Renal Replacement Therapy: Who, When, Why, and How, CHEST 2019
Renal replacement therapy in ICU, J Anaesthesiol Clin Pharmacol. 2012
The ultrafiltration coefficient: this old ‘grand inconnu’ in dialysis, NDT 2013
Choosing a dialyzer: What clinicians need to know, Hemodialysis International 2018
Prescription of CRRT: a pathway to optimize therapy, Annals of Intensive Care, 2020
-
-