#21 Feeding in Critical Illness w/ Dr. Paul Wischmeyer
On this MEGAsode of Critical Care Time, Cyrus & Nick are joined by world-renowned expert in ICU nutrition, Dr. Paul Wischmeyer (X: Paul_Wischmeyer & IG: paul_wischmeyermd) to discuss all things ICU nutrition. This episode is highly fortified with practice changing pearls from soup to nuts! In addition to getting to know who Paul is and why he does what he does, we demystify metabolic carts, talk about protein needs and metabolism in the critically ill, discuss steroids and other supplements - all while dispelling some major ICU myths regarding gastric residuals, TPN and more. Grab a healthy snack, sit back and get ready to enjoy some remarkable content in an oft overlooked field in medicine!
Quick Take Home Points:
ICU patients receive less than 50% of the prescribed calories and inadequate protein, leading to worse outcomes.
Volume and bolus based enteral nutrition can help correct inadequate delivery of nutrition.
There are misconceptions and myths surrounding critical care nutrition that need to be addressed:
Feeding patients on vasopressors and neuromuscular blockers is safe and beneficial in most cases.
Gastrointestinal residuals should not be routinely checked in medical ICU patients.
Prone positioning is not a contra-indication to feeding.
Anabolic agents, such as testosterone, can help patients gain muscle and improve their overall recovery.
Comprehensive rehabilitation programs are essential for addressing both physical and cognitive recovery.
Indirect calorimetry (a.k.a. metabolic cart) can help personalize nutrition and may be associated with reduced mortality.
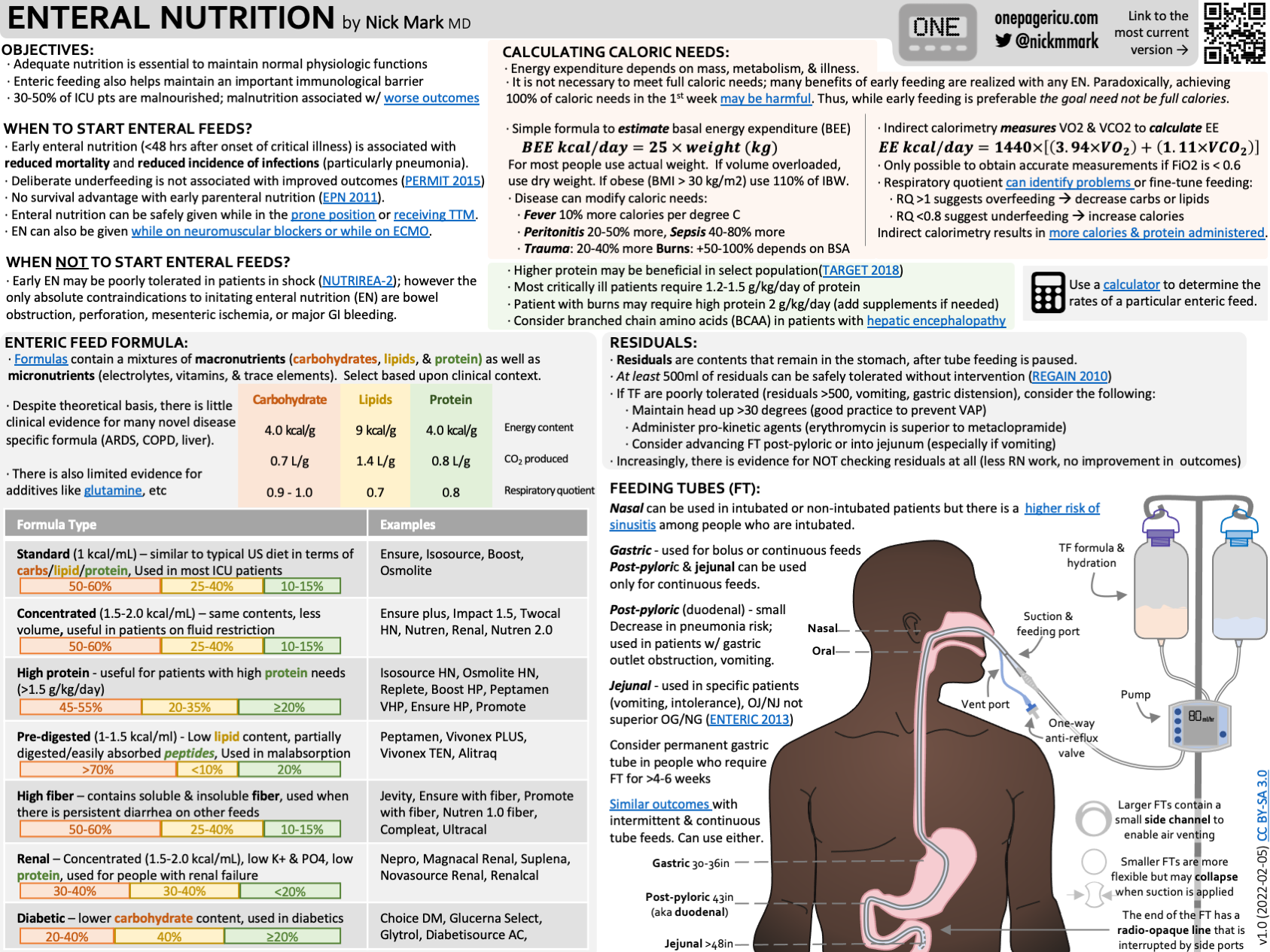
Infographic:
Infographic summarizing the key take away points!
Show Notes:
“Imagine if a gram of vancomycin was ordered but only 500 mg was given for 10 days? That would be malpractice. But this happens routinely everywhere with nutrition”
Inadequacy of nutrition in people with critical illness
We do an abysmal job providing nourishment to people with critical illness:
In the first 12 days of critical illness, ICU patients receive less than 50% of caloric need.
30-50% of ICU patients are malnourished.
It is recommended that ICU patients receive 1.5 g/kg of protein but less than half ICU patients actually receive the recommended protein. We average 0.6 gm/kg which is roughly a third the prescribed amount of protein. This likely contributes to muscle catabolism and ICU acquired weakness
Patients who do receive appropriate nutrition have better outcomes, both within the ICU and afterwards:
Shorter ICU and hospital LOS
Less time on ventilators
Lower hospital mortality
Higher quality of life after discharge
In both RCTs and large observational studies, initiating nutrition early (within 72 hours of admission) is associated with improved outcomes:
Shorter ICU length of stay
Shorter duration of mechanical ventilation
Lower mortality
Importantly overfeeding and underfeeding is also associated with worse outcomes
Why do we do such an inadequate job providing nutrition to people with critical illness?
Many operational reasons:
Inappropriate delays in starting nutrition
Providing too much or too few calories
Inappropriate holding of enteral nutrition (EN)
Perseverating about gastric residuals
Delays after G-tube placement
Root causes:
Inadequate education!
75% of US medical schools don’t teach any clinical nutrition!
Incorrect assumptions about caloric needs
The equations used to calculate caloric requirements are only accurate about 50% of the time.
Empirical measurements (e.g. metabolic carts) are superior to estimates, and often lead to changes in prescribed nutrition.
ICU OnePager infographic about enteral nutrition in the ICU.
How to providing early & adequate nutrition in the ICU
Feeding is not a “day shift problem”
How can you feed a patient?
In general, start slow and escalate gradually over the first few days
Martha Van Zandt paper: <0.8 gm/kg of protein is associated with better outcomes in the first 3 days.
Patients who are on CRRT may benefit from more calories and higher protein sooner. (CRRT causes patients to waste amino acids)
Determine caloric needs (use a metabolic cart if you can!)
Probably reasonable to provide 25% on day one, 50% on day two, 75% on day three and then get up to 100% by day 4 or 5
Mitochondrial dysfunction in acute critical illness precludes optimal utilization of nutrition in the first ~72 hours of disease, which is why a more restrictive strategy up front in sensible
Protein: Dr. Wischmeyer recommends starting at 0.8 gm/kg in the first 3-4 days days, then advancing to 1.2-1.5 in most patients, and up to 2.0 or more in those that are hypercatabolic or are on CRRT for example.
CRRT wastes around 30% of amino acids which impairs muscle protein synthesis
Goal: Ramp up calories AND protein
Remember that too much protein (>2.2 gm/kg/day) is likely harmful in people with AKI. (EFFORT protein trial)
Make adjustments based on metabolic cart data - this will account for physical therapy expenditures, ebbs and flows of disease
Early EN is associated with reduced risk of postoperative infections
A recent RCT compared Early vs late Supplemental Parenteral Nutrition (SPN) in patients who underwent abdominal surgery.
Early SPN was began on day 3, Late SPN began on day 7
The early SPN group had significantly fewer nosocomial infections compared with the late SPN group (8.7% 18.4%)
NNT = 10.3 to prevent one nosocomial infection
Consider early parenteral nutrition in people who are undergoing abdominal surgery and are at high risk for intolerance.
When do we start?
It is safe to feed patients who are on low dose vasopressors. In fact, early enteral nutrition was associated with reduced mortality in one study of patients on low and medium dose vasopressors.
In order to qualify for early enteral nutrition a patient should be hemodynamically stable - this doesn’t mean they are completely off pressors - but they are on a relatively consistent dose and their clinical status is not actively in flux.
Lactate normal or improving
Fluid resuscitation completed
If so, start trophic feeds at 10-15 cc/hr and based on the patient, consider going to the goal rate within 24-48 hours!
What to do if my patient is “unstable”?
If a patient becomes unstable EN or parenteral nutrition (PN) can be reduced back to trophic levels or stopped
If BUN is on the rise, should consider dropping feeds to at least 1gm/kg - this is concerning for an increase in toxic, unmeasured metabolites
In an acutely worsening patient, remember GI blood flow drops and their ability to use the calories effectively worsens resulting in increased risk for gut ischemia and production of toxic metabolites
Consider trophic parenteral nutrition if you cannot feed the gut within 48 hours (ex - post bowel surgery patient)
Dr. Wischmeyer recommends 500 cal/day, ramped up to goal as able - similarly to how EN is ramped up
Where to feed? Gastric vs post-pyloric?
Gastric is generally preferred - this is physiologic
Can only do bolus feeding to the stomach
Post pyloric vs gastric - somewhat controversial. Meta-analysis suggest that post-pyloric FT may be associated with reduced pneumonia risk and improved nutritional delivery however not all studies agree on this point & placement may be technically challenging
Patients with profound gastroparesis (ex: those on GLP-1 agonists, poorly controlled DM) may benefit from post-pyloric tubes
Volume-based strategy
Determine total volume needed in 24 hours, use this to ramp up feeds intermittently to account for time off the pump (during procedures, imaging, etc.).
Instead of targeting an hourly rate target a total daily volume of TF to deliver.
The PEP uP Trial found a 12-15% increase in protein delivered without adverse safety events.
Potential benefit of bolus feeding
As humans, we do not eat continuously so feeding patients continuously is likely non-physiologic.
“Muscle full effect” - muscle protein synthesis is stimulated by peaks and valleys in serum amino acid levels. Thus there may be advantages to simulating a “fed” and “fasted” state using bolus nutrition.
How: 200-300cc every 3-4 hours. Can increase to “catch up” for missed feeds.
There are non-nutritive benefits to feeding in critically illness
Early feeding is not just about delivery of calories, protein, and other nutrients. The act of feeding is likely highly beneficial in most patients. Enteral nutrition:
Preserves microbiome
Maintains gut permeability
Has Anti inflammatory effects via vagally mediated gut signaling
May have modulatory effects. Lymph toxicity mitigation/reduction - which can theoretically reduce the incidence of ARDS given that lymph drainage via the thoracic duct drains to the pulmonary lymphatics and thus toxic lymph drainage may contribute to the development of ARDS
Using Metabolic Carts
Instead of estimating caloric needs using a reference equation, indirect calorimetry (a.k.a. “a metabolic cart”) actually measures energy expenditure by measuring the body's oxygen consumption and carbon dioxide production using a computerized instrument. This permits more precise nutrition to be delivered and avoids over and underfeeding.
Newer-iterations of metabolic carts are much more portable and easier to use. They can measure O2 and CO2 either from the ventilator circuit or using a hood in patients not on mechanical ventilation.
Easily implemented on ventilated patients, minimal nursing / RT burden.
Reference equations are quite unreliable at predicting actual caloric requirements. For example, among people with severe COVID there was a significant discrepancy between IC measured and estimated caloric requirements.
A recent meta-analysis suggests that indirect calorimetry guided nutrition was associated with reduced mortality & proponents argue that use of IC should be standard of care in the ICU.
Sources of error:
CRRT does not impact results significantly
Significant air leaks, FiO2 > 70% will mess up your results
Demonstration of the use of a modern Q-NRG+ indirect calorimeter.
Myth-busting some pervasive myths about ICU Nutrition
TPN is NOT associated with increased risk of Candidemia or other infections
4 large RCTs
NUTRERIIA 2
CALORIES
Early SPN
PN Trial
Why?
Better techniques for sterile line placement
Increased focus on managing hyperglycemia
PN and EN can be used TOGETHER
Combining EN and PN is a good way to realize the benefits of trophic feeds in patients who are unable to receive their complete nutritional demands via their GI tract.
Checking residuals is NOT necessary or appropriate - especially in MICU patients
Consider checking every 6-8 hours in major abdominal surgery patients, burn patients and the number you look for is >500cc
Can be an early marker of sepsis, worsening disease
Feeding SHOULD occur even if a patient is on pressors!
A large Japanese observational study with 52,000 patients found that early enteral nutrition was associated with a reduction in mortality in ventilated adults treated with low- or medium-dose (but NOT high dose) norepinphrine
Note: if the patient is worsening, consider dropping to a trophic rate or stopping until stability is restored - whether it’s EN or PN
Tube feeding does NOT need to stop when patients are prone
Patients who are prone DO NOT need post-pyloric tubes
Tube feeding does NOT need to stop when patients are on neuromuscular blockers
In fact, enteral feeding is associated with decreased mortality in patients who are receiving neuromuscular blockers in one large observational study.
You should TRY to feed those undergoing TTM - may not be successful due to gastroparesis, may need less than those who are not being cooled.
We do NOT need to routinely wait 24 hours after G-tube placement to begin feeds
ASPEN guidelines: 4 hours
Listen to the surgeon/proceduralist on this, but routinely waiting 12+ hours is inappropriate. If your institution is waiting 24 hours to start using a G-tube you need to change your policies!
Role for Supplements in Critical Care Nutrition
Nutritional supplements is a largely unregulated, multi-billion dollar industry. Many low quality studies of supplements are published every year, but few are robust, reproducible, and applicable to people with critical illness. Avoid drawing inferences about the role of supplements from low quality studies performed in people not experiencing critical illness.
Based on high quality RCTs performed in people with critical illness, we can make several observations about micronutrients.
Continuous Renal Replacement Therapy (CRRT) in a major sink for many nutrients. Deficiencies of these micronutrients can cause symptoms that can prolong critical illness and adversely affect long term outcomes. Worse most of of these deficiencies are non-specific so it is easy to miss:
Copper deficiency - life threatening pancytopenia, permanent neuromuscular weakness
B6 deficiency - obtundation/encephalopathy
Carnitine deficiency - weakness
Selenium deficiency - weakness, fatigue
Thiamine deficiency - many symptoms, lactic acidosis
Amino acids - may need to provide >2 gm/kg/day of protein to people on CRRT
Glutamine
Although it is not an essential amino acid, severe deficiencies of glutamine have been observed in people with critical illness. Parenteral nutrition in the US does NOT have glutamine and several meta-analyses suggested reduced mortality with glutamine supplementation. Thus glutamine supplementation has been an area of intense research interest.
The REDOX trial found no overall benefit to glutamine supplementation in critical illness, however inadequate dose in the sickest patients - those receiving CRRT - may have biased this study towards null.
Testosterone/Oxandrolone
Many patients develop significant weakness during critical illness. Anabolic resistance is suspected to be a significant contributor.
Used often in burn ICUs - specifically oxandrolone (purely anabolic, not virilizing)
Testosterone
Increased clot, heart attack, stroke... this is related to the PO formulation due to the aromatized metabolite
Large, JAMA IM study (Kaiser) - IM supplementation in deficient patients REDUCES CV risk significantly
Intermountain health (9000 patients) - no bad outcomes
Dr. Wischmeyer says:
Consider checking Testosterone levels in high risk patients - those that are weak, expected to become weak, or already sarcopenic
Treat at <250-300 ng/dL
Don’t need total and free - we aren’t assessing the intricacies of testosterone metabolism in these patients
Check again in 1 week after treatment (half-life 9 days)
Treatment in a 70kg male is 200mg IM every 2 weeks
Goal 500-600 ng/dL based on urologic guidelines
Goal 350-500 ng/dL in females
Duration: 6 months or less
Adjust based on findings
Creatine
This is often thought of as “an ATP regenerator” (phosphocreatine is a rapidly mobilizable reserve of high-energy phosphates)
Not studied in ICU populations robustly
Significant data in non-critically ill patients supporting role in muscular performance / power generation
Dr. Wichmeyer will start in patients during their ICU-based rehab
Hydroxymethylbutyrate (HMB)
MTor agonist. The mechanisms of human muscle catabolism are incompletely understood, particularly in critical illness, however it is believed that HMB stimulates muscle synthesis.
Several studies have found reduced sarcopenia in elderly patients with HMB supplementation, however trials have found inconsistent results among people with critical illness.
The BOOST trial is ongoing to study HMB supplementation
Branch chain amino acids (at night)
Increased muscle mass development / utilization during sleep
Whey protein
Best form of protein supplementation that can be used in post-ICU rehabbing patients
Vitamin-D
Supports bone health, deficiency can lead to fatigue and muscle weakness
Exercise, muscle mass and critical illness
Sarcopenia: One of the most profound predictors of morbidity and mortality
As we age, we need more protein and we need to exercise more to build/maintain muscle mass
Cancer study: more muscle mass before chemo, patients lived 2 years longer than those who were sarcopenic going into treatment
Critically ill elders: Can lose 10% of muscle mass in three days of their illness
Anabolic agents, such as testosterone, can help patients gain muscle and improve their overall recovery.
Comprehensive rehabilitation programs are essential for addressing both physical and cognitive recovery.
Audio
Video
-
Wischmeyer PE, et al Personalized nutrition therapy in critical care: 10 expert recommendations. Crit Care. 2023 (High yield summary of the topic)
Wischmeyer PE. Overcoming challenges to enteral nutrition delivery in critical care. Curr Opin Crit Care. 2021 (Overcoming challenges and barriers to EN covers many of the myths discussed!)
Wischmeyer PE. Enteral Nutrition Can Be Given to Patients on Vasopressors. Crit Care Med. 2020
Ohbe H et al Differences in effect of early enteral nutrition on mortality among ventilated adults with shock requiring low-, medium-, and high-dose noradrenaline: A propensity-matched analysis. Clin Nutr. 2020 (Observational trial showing mortality reduction of early EN on vasopressors)
Reduced Complications better outcomes with early EN on paralytics observational study in CCM:
Ohbe H et al Early Enteral Nutrition in Patients Undergoing Sustained Neuromuscular Blockade: A Propensity-Matched Analysis Using a Nationwide Inpatient Database. Crit Care Med. 2019
McNelly AS et al Effect of Intermittent or Continuous Feed on Muscle Wasting in Critical Illness: A Phase 2 Clinical Trial. Chest. 2020
Bear DE, Hart N, Puthucheary Z. Continuous or intermittent feeding: pros and cons. Curr Opin Crit Care. 2018
Zusman O et al Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 2016 (Key How Much to feed in 1st week article - often shown and cited for 70% of measured energy expenditure from Metabolic Cart:)
Poor Performance of Predictive Equations for energy prediction – WHY WE ALL NEED METABOLIC CARTS/INDIRECT CALORIMETER’s
Zusman O et al. Predictive equations versus measured energy expenditure by indirect calorimetry: A retrospective validation. Clin Nutr. 2019
Reduced Mortality with Indirect Calorimeter Use in ICU
Duan JY, Zheng WH, Zhou H, Xu Y, Huang HB. Energy delivery guided by indirect calorimetry in critically ill patients: a systematic review and meta-analysis. Crit Care. 2021 Feb 27;25(1):88. doi: 10.1186/s13054-021-03508-6. PMID: 33639997; PMCID: PMC7913168.
New paper describing nee generation metabolic cart validation and use:
Oshima T, Delsoglio M, Dupertuis YM, Singer P, De Waele E, Veraar C, Heidegger CP, Wernermann J, Wischmeyer PE, Berger MM, Pichard C. The clinical evaluation of the new indirect calorimeter developed by the ICALIC project. Clin Nutr. 2020 Oct;39(10):3105-3111. doi: 10.1016/j.clnu.2020.01.017. Epub 2020 Jan 31. PMID: 32046881.
Our data in COVID showing inaccuracy of predictive equations in ICU vs. metabolic cart:
Niederer LE, Miller H, Haines KL, Molinger J, Whittle J, MacLeod DB, McClave SA, Wischmeyer PE. Prolonged progressive hypermetabolism during COVID-19 hospitalization undetected by common predictive energy equations. Clin Nutr ESPEN. 2021 Oct;45:341-350. doi: 10.1016/j.clnesp.2021.07.021. Epub 2021 Aug 3. PMID: 34620338; PMCID: PMC8328525.
Guidelines for how to use indirect calorimetry in ICU
Wischmeyer PE et al, Indirect Calorimetry is Essential for Optimal Nutrition Therapy in the ICU, Nutr Clin Pract. 36:275-281, 2021
Role of Anabolic Resistance and Muscle in ICU
Morton RW, Traylor DA, Weijs PJM, Phillips SM. Defining anabolic resistance: implications for delivery of clinical care nutrition. Curr Opin Crit Care. 2018 Apr;24(2):124-130. doi: 10.1097/MCC.0000000000000488. PMID: 29389741.
Why we should ramp up protein in ICU over first few days-
Koekkoek et al, Clin Nutr. 38:883-890, 2019
Real World Data on how Early EN (in first 3 days) reduce mortality and complications from large Premier database:
Haines KL, Ohnuma T, Grisel B, Krishnamoorthy V, Raghunathan K, Sulo S, Kerr KW, Besecker B, Cassady BA, Wischmeyer PE. Early enteral nutrition is associated with improved outcomes in critically ill mechanically ventilated medical and surgical patients. Clin Nutr ESPEN. 2023 Oct;57:311-317. doi: 10.1016/j.clnesp.2023.07.001. Epub 2023 Jul 16. PMID: 37739674.
Key Trials Showing TPN Does Not Increase Infection Risk:
1. Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, Davies AR, O'Leary M, Solano T, Peake S; Early PN Investigators of the ANZICS Clinical Trials Group. Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA. 2013 May 22;309(20):2130-8. doi: 10.1001/jama.2013.5124. PMID: 23689848.
2. Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, Bellingan G, Leonard R, Mythen MG, Rowan KM; CALORIES Trial Investigators. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014 Oct 30;371(18):1673-84. doi: 10.1056/NEJMoa1409860. Epub 2014 Oct 1. PMID: 25271389.
3. Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, Thibault R, Pichard C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013 Feb 2;381(9864):385-93. doi: 10.1016/S0140-6736(12)61351-8. Epub 2012 Dec 3. PMID: 23218813.
4. Reignier J, Boisramé-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, Argaud L, Asehnoune K, Asfar P, Bellec F, Botoc V, Bretagnol A, Bui HN, Canet E, Da Silva D, Darmon M, Das V, Devaquet J, Djibre M, Ganster F, Garrouste-Orgeas M, Gaudry S, Gontier O, Guérin C, Guidet B, Guitton C, Herbrecht JE, Lacherade JC, Letocart P, Martino F, Maxime V, Mercier E, Mira JP, Nseir S, Piton G, Quenot JP, Richecoeur J, Rigaud JP, Robert R, Rolin N, Schwebel C, Sirodot M, Tinturier F, Thévenin D, Giraudeau B, Le Gouge A; NUTRIREA-2 Trial Investigators; Clinical Research in Intensive Care and Sepsis (CRICS) group. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet. 2018 Jan 13;391(10116):133-143. doi: 10.1016/S0140-6736(17)32146-3. Epub 2017 Nov 8. PMID: 29128300.
New Trial Showing REDUCED infections with early TPN in major surgery with early TPN use in JAMA Surgery
Gao X, Liu Y, Zhang L, Zhou D, Tian F, Gao T, Tian H, Hu H, Gong F, Guo D, Zhou J, Gu Y, Lian B, Xue Z, Jia Z, Chen Z, Wang Y, Jin G, Wang K, Zhou Y, Chi Q, Yang H, Li M, Yu J, Qin H, Tang Y, Wu X, Li G, Li N, Li J, Pichard C, Wang X. Effect of Early vs Late Supplemental Parenteral Nutrition in Patients Undergoing Abdominal Surgery: A Randomized Clinical Trial. JAMA Surg. 2022 May 1;157(5):384-393. doi: 10.1001/jamasurg.2022.0269. PMID: 35293973; PMCID: PMC8928091.
New data for use of New Fish Oil (SMOF Lipids) reduces UTI infections and length of stay in adults and children in ICU and hospital getting TPN:
Adults: Haines KL, Ohnuma T, Trujillo C, Osamudiamen O, Krishnamoorthy V, Raghunathan K, Wischmeyer PE. Hospital change to mixed lipid emulsion from soybean oil-based lipid emulsion for parenteral nutrition in hospitalized and critically ill adults improves outcomes: a pre-post-comparative study. Crit Care. 2022 Oct 18;26(1):317. doi: 10.1186/s13054-022-04194-8. PMID: 36258222; PMCID: PMC9578223.
Pediatrics: Haines KL, Ohnuma T, Hornik CD, Grisel B, Leraas H, Trujillo CN, Krishnamoorthy V, Raghunathan K, Wischmeyer PE. Change to Mixed-Lipid Emulsion From Soybean Oil-Based Lipid Emulsion in Pediatric Patients. JAMA Netw Open. 2023 Sep 5;6(9):e2332389. doi: 10.1001/jamanetworkopen.2023.32389. PMID: 37669048; PMCID: PMC10481238.
NEW ASPEN Guidelines saying early PN or early EN is equally safe and can be started interchangeably:
J Parenter Enteral Nutr. 46: 12– 41, 2022.
Key new data on ~ 90% of patients on CRRT developing significant micronutrient deficiencies:
Fah M, Van Althuis LE, Ohnuma T, Winthrop HM, Haines KL, Williams DGA, Krishnamoorthy V, Raghunathan K, Wischmeyer PE. Micronutrient deficiencies in critically ill patients receiving continuous renal replacement therapy. Clin Nutr ESPEN. 2022 Aug;50:247-254. doi: 10.1016/j.clnesp.2022.05.008. Epub 2022 May 23. PMID: 35871932.
Review on CRRT vitamin / nutrient management:
Berger MM, Broman M, Forni L, Ostermann M, De Waele E, Wischmeyer PE. Nutrients and micronutrients at risk during renal replacement therapy: a scoping review. Curr Opin Crit Care. 2021 Aug 1;27(4):367-377. doi: 10.1097/MCC.0000000000000851. PMID: 34039873; PMCID: PMC8270509.
Large RCT on why we recommend use of oral nutrition supplements with HMB or just HMB use:
Deutz NE, Matheson EM, Matarese LE, Luo M, Baggs GE, Nelson JL, Hegazi RA, Tappenden KA, Ziegler TR; NOURISH Study Group. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin Nutr. 2016 Feb;35(1):18-26. doi: 10.1016/j.clnu.2015.12.010. Epub 2016 Jan 18. PMID: 26797412.
HMB reversing muscle loss from Bedrest paper:
Deutz NEP, et al. Clin Nutr 2013; 32: 704-712.
Testosterone Reducing CV Event (MI) and stroke risk when replaced with IM doses in JAMA Internal Medicine
Cheetham TC, An J, Jacobsen SJ, et al. Association of Testosterone Replacement With Cardiovascular Outcomes Among Men With Androgen Deficiency. JAMA Intern Med. 2017;177(4):491–499. doi:10.1001/jamainternmed.2016.9546
Review article on use of Anabolic agents (testosterone/oxandrolone) and exercise in ICU
Wischmeyer PE, Suman OE, Kozar R, Wolf SE, Molinger J, Pastva AM. Role of anabolic testosterone agents and structured exercise to promote recovery in ICU survivors. Curr Opin Crit Care. 2020 Oct;26(5):508-515. doi: 10.1097/MCC.0000000000000757. PMID: 32773614; PMCID: PMC8367823.
Review articles on use of CPET testing and exercise prescription in ICU patient recovery:
Molinger J, Pastva AM, Whittle J, Wischmeyer PE. Novel approaches to metabolic assessment and structured exercise to promote recovery in ICU survivors. Curr Opin Crit Care. 2020 Aug;26(4):369-378. doi: 10.1097/MCC.0000000000000748. PMID: 32568800; PMCID: PMC8104451.
Whittle J, San-Millán I. Objective assessment of metabolism and guidance of ICU rehabilitation with cardiopulmonary exercise testing. Curr Opin Crit Care. 2021 Aug 1;27(4):390-398. doi: 10.1097/MCC.0000000000000843. PMID: 33973897.
Our New NIH funded trial using Exercise Prescription with CPET testing for COVID-19 patients with great applicability to ICU patients:
REmotely Monitored, Mobile Health Supported Multidomain Rehabilitation Program With High Intensity Interval Training for COVID-19 (REMM-HIIT-CoV)
https://clinicaltrials.gov/study/NCT05218083?term=REMM-HIIT&rank=2
-
REDOX (glutamine in critical illness)
NUTRERIIA 2
CALORIES
EFFORT (high protein trial)
PEP uP
-