#22 Bronchoscopy Emergencies w/ PulmPEEPs
Like that time the Jetsons met the Flintstones or the more recent colab between Lululemon and Peloton, join us for an epic pairing between Critical Care Time hosts Cyrus & Nick and the PulmPEEPS - Drs. Dave Furfaro and Kristina Montemayor. On this show we use a case based approach to answer the question: How can a bronchoscope save your @$$ in the ICU and beyond? We take a practical look at airway bleeds, trach emergencies and so much more with our friends from PulmPEEPs! Make sure to give this a listen and let us know what you think!
Our first crossover episode between Critical Care Time and Pulm PEEPs
Quick Take Home Points:
Bronchoscopy is an important skill for any clinician caring for the critically ill - or those who could become critically ill! The bronchoscope can facilitate advanced diagnostics, confirm airway placement, remedy a trach dislodgement and be essential in clearing the airway of a patient in extremis!
Remember: Critical care is a team sport. Airway emergencies especially can be stressful and often require numerous hands on deck. Check your ego at the door, call for back-up and focus on the task at hand.
Diagnostic Bronchoscopy: In certain situations, the bronchoscope can be used to obtain biopsies, cultures and cell differentials to assist in diagnosing conditions such as DAH and AEP. These are situations where making the diagnosis is often critical as it has great potential to shift if not completely alter the treatment course for a patient. All efforts should be made to avoid purely diagnostic bronchoscopies in actively tenuous patients, although, there are times when we need to weigh the risks and benefits of obtaining the answer versus empiric therapies.
Bronchoscopy and Difficult Airways: Consider using the bronchoscope to perform awake, fiber optic intubations in patients you are reluctant to paralyze. You can also easily use a bronchoscope to confirm ET tube placement. Need a bougie with a camera? You can always use a DISPOSABLE bronchoscope to confirm location and perform an exchange if you have a pair of trauma shears available… just DON’T do this to you 40K durable scopes!
Tracheostomy Emergencies: Have a bronchoscope to deal with a fresh trach that gets dislodged is clutch! If the scope is readily available you can use it to either navigate the stoma site, avoid false lumens and re-secure a trach OR use it to assist in your intubation from above.
Foreign Bodies: The bronchoscope is the ultimate tool for getting down in the airways and pulling out stuff that ain’t supposed to be there! Make sure you have the right forceps, snares, baskets etc ready to go as you never know what you’ll see. It’s a good idea to use a therapeutic scope (bigger working channel) to make your life easier when it comes to passing tools in and out of the scope.
Airway Clearance: Whether it's a bleed or mucus - the bronchoscope can be your friend! We go from soup to nuts on airway bleeds in episode 14 - check that out for all the deets! When it comes to mucus plugs - they can be a big problem when they cause lobar collapse, especially in a tenuous patient. Again, make sure you grab a therapeutic scope for these cases! Note - the scope may be an appealing option, but this does NOT clear distal airways very effectively… that’s what chest physiotherapy and all your other airway clearance interventions are for! One other point - Sometimes these patients are very tenuous and require a lot of support BECAUSE of their need for airway clearance… You cannot wait for these patients to be more stable because they need the intervention NOW in order to achieve stability!
Show Notes:
Utility of bronchoscopy in people with critical illness
Bronchoscopy can be both diagnostic and therapeutic; both are potentially lifesaving.
General situations where bronchoscopy is useful in the ICU:
Placing (or confirming placement of) an endotracheal tube or tracheostomy tube
Removing a foreign body or mucous plugs from the lungs
Localizing the source of pulmonary hemorrhage or performing interventions to stop/contain the bleed
Diagnosing certain rare conditions, particularly those where the diagnosis can substantially change management (e.g. DAH, AEP, rare infections, etc).
Proficiency with bronchoscopy is important to realize the benefits. Simply “having the equipment” is insufficient, regular practice/simulation is essential
Anesthesiologists, emergency physicians, and other specialists may have limited experience with bronchoscopy in training. Even experienced pulmonologists, who may be good at diagnostic bronchoscopy often have limited experience deploying bronchial blockers, using retrieval baskets, etc.
Remember: “People don’t rise to the occasion, they sink to the level of their training.”
If you haven’t regularly practiced with a bronchoscope, you are not going to be able to use it effectively under stress when performing high acuity low occurrence (HALO) procedures such as in emergent airways, deploying bronchial blockers, retrieving foreign bodies, etc.
Practice practice practice: High fidelity bronchoscopy simulators are available. Low cost bronchoscopy simulators (e.g. 3D printed DIY) are available.
Difficult Airways
Two broad situations where a bronchoscope is generally used:
Awake intubation in the anticipated difficult airway (e.g. someone with abnormal anatomy, airway tumor, etc)
Rescue method in the unanticipated difficult airway (e.g. very anterior cords, difficulty with Bougie, etc)
Nasal vs Oral approach:
Oral approach is usually used in an unanticipated difficult airway
Nasal approach: More common if performing an awake intubation. Nasal is often better tolerated however epistaxis can make a difficult airway almost impossible.
Sedation strategy:
Full topicalization: lidocaine vs cocaine (equally effective and lidocaine is normally preferred, however the vasoconstriction action of cocaine may be helpful in preventing epistaxis).
Which types of topicalization work best?
Spray as you go w/ or w/o and atomizer
Nebulization (maybe better? maybe)
Gurgling (Nick: from personal experience lidocaine is super gross)
Remember total dose of lidocaine: < 8 mg/kg
Ketamine
Ideal because it’s dissociative and analgesic, maintains respiratory drive and (maybe) airway reflexes
Consider scopolamine patch to reduce oral secretions
Dexmedetomidine
Great adjunct
One vs two operator
Especially in unanticipated difficult airways; the second operator can use VL/DL to facilitate visualization of the vocal cords.
Second operator can also be preparing for a surgical airway.
Equipment considerations:
Preload the endotracheal tube onto the bronchoscope. Use the bronchoscope as a bougie to guide the ETT through the vocal cords.
Suction! You want two - one connected to the bronch and one connected to a yankuer.
Disposable vs “good” scope
Remember to load the tube first!
Also remember to lube the tube!
Approach to Tracheostomy Emergencies from ICU OnePager
Tracheostomy troubleshooting
Similarly to intubation, bronchoscopy can be very useful to confirm placement
Mechanics are similar to above
Goal is to avoid inadvertent placement of the tracheostomy tube into the soft tissues of the neck and to avoid putting air into those tissues (false lumen).
Advanced trick for exchanging tubes: You can use a disposable bronchoscope to exchange tubes: you can get it in, confirm placement, then cut it with trauma shears! Now you can slide the old tube out and put a new one in. (Don’t try this on a $40,000 fiberoptic bronchoscope!)
Ideally you should load the ETT onto the bronchoscope in advance (red arrow). If necessary however, you can cut the ETT and turn the disposable bronchoscope into a improvised exchange catheter. This technique is very useful for exchanging tracheostomy tubes.
Foreign Body Removal from airways
Bronchoscopy is invaluable for both diagnosis and treatment of foreign body aspirations.
Most commonly these aspirations are food (nuts, seeds, etc), teeth, pills, etc
Intubated vs awake
Intubated is harder in many cases: no cough to help, hard to get foreign body out of the ETT.
Flexible vs rigid
Most objects can be retrieved using flexible bronchoscope; however 15-20% require rigid bronchoscopy
Flexible can reach smaller foreign bodies that are lodged more distally.
Rigid bronchoscopy is usually done if flexible bronchoscopy fails; an interventional pulmonologist wielding a rigid is superior but more invasive (requires GA)
Many different retrieval devices; technique depends on what equipment is available.
Mucous Plugs & Lobar collapse
Presentation can be subtle or dramatic.
Bronchoscopy can remove mucous plugs and help re-expand collapsed lung areas, which is potentially life saving.
Additionally, bronchoscopy can permit diagnosis of tracheal bronchus (bronchus sui)
Pig bronchus - 1-3% of people - have a RUL bronchus that comes off the trachea.
Often presents with RUL collapse in an intubated person.
Suction considerations and bronchoscope size
Remember that suctioning force is highly dependent (i.e. radius raised to the fourth power!) upon the working channel size. Use the largest size bronchoscopy possible when suctioning.
Remember that other interventions: regular inline suctioning, chest PT, adequate hydration, mucolytics are also important to prevent recurrent mucous plugging.
Recognizing the patterns of lobar collapse on chest radiographs is important:
Radiographic patterns of lobar collapse, from ICU OnePager
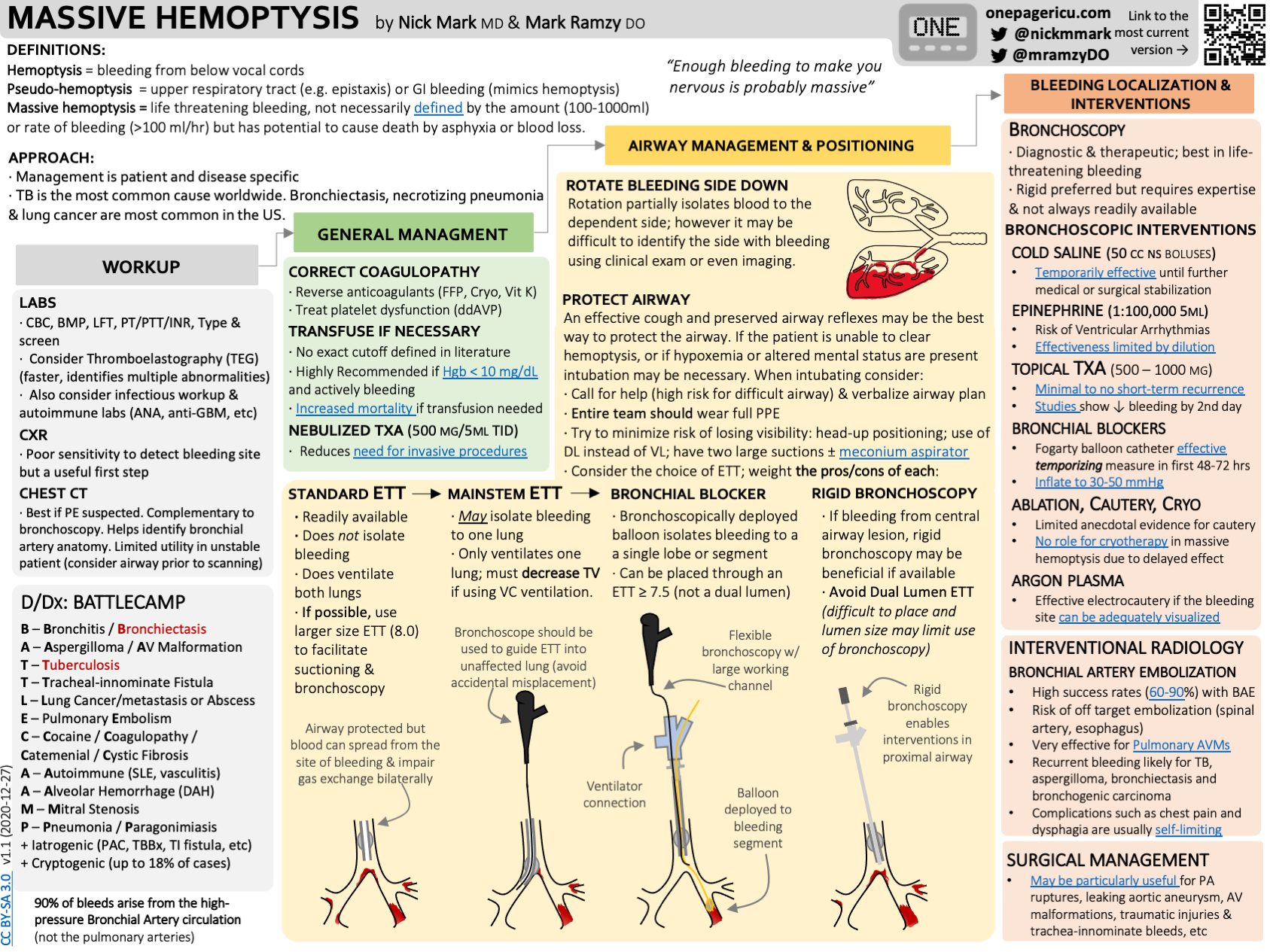
Localization & Isolation of Pulmonary Hemorrhage
Pre-bronch interventions
Stabilization
Nebulized TXA
Bad side down → counter-intuitive because shifting blood flow, but also the goal is to protect the non-bleeding lung.
etc
Bronch can localize the bleeding site. Bronch can also perform interventions such as:
Cold saline
Epinephrine 1:100,000
Bronchial blockers - comparison of types
CRE balloon
Fogarty
Cryo probe - great for removing clots
Delivering ETT to contralateral side → single lung ventilation
Etc
See our episode on pulmonary hemorrhage for more information!
Approach to Massive Hemoptysis from ICU OnePager
Making “bronchoscopy only” diagnoses
Diffuse Alveolar Hemorrhage (DAH)
Finding: Increasingly bloody returns on serial lavages
Infections not covered by empiric therapies:
Invasive fungal infection (e.g. mucor), azole resistant fungi (C glabrata)
Rare/unusual infections (PJP, histoplasmosis, etc)
Infection mimics:
Acute eosinophilic pneumonia (AEP) and chronic eosinophilic pneumonia (CEP)
Finding: eosinophils > 20%
E-Cigarette Vaping Associated Lung Injury (EVALI)
Foamy lymphocytes
Organizing Pneumonia
Others
Remember to always send a cell count on a BAL! And cytology!
How often does bronchoscopy change management? Surprisingly often!
A study of how often bronchoscopy changes management in an oncology population. 500+ patients with AML or high grade myeloid neoplasms who underwent bronchoscopy at one center over 5+ years.
1) an unexpected diagnosis was made and followed by a management change (as the most rigorous estimate of utility)
13% of the time a diagnosis was only made because of bronchoscopy which changed management
2) the post-bronchoscopy diagnosis was discordant from the leading diagnosis considered before this procedure and was followed by a management change
48% of the time pre and post procedure leading diagnoses were different
26% of the time the change in leading diagnosis led to a change in therapy
3) a change in management was made following bronchoscopy regardless of whether the diagnosis was expected or considered.
32% escalation of antibiotics
30% de-escalation of antibiotics
9% addition of steroids
2% mold → surgery
Remember that in critically ill patients whose symptoms are unexplained or failing to resolve with therapy, diagnostic flexible bronchscopy can provide useful insights.
Audio
Video
-
Patolia S, Farhat R, Subramaniyam R. Bronchoscopy in intubated and non-intubated intensive care unit patients with respiratory failure. J Thorac Dis. 2021
Seghal et al, Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature, Respiratory Care 2015
Ma, W. et al. Application of flexible fiberoptic bronchoscopy in the removal of adult airway foreign bodies. BMC Surgery 2020
Wahidi MM, et al, American College of Chest Physicians Consensus Statement on the Use of Topical Anesthesia, Analgesia, and Sedation During Flexible Bronchoscopy in Adult Patients CHEST 2011
Mark, N.M. Crowning achievement: a case of dental aspiration, Radiology Case Reports 2015
Buckley, S.A. & Mark, N.M. Diagnostic utility of bronchoscopy in adults with acute myeloid leukemia and other high-grade myeloid neoplasms. Leukemia & Lymphoma, 2019
-
-